Why patients drop out of weight management trials and what you can do about it

Retention in obesity and weight-management trials remains a significant challenge, with dropout rates reaching 30–65% within the first year.1–5 Retention is about more than just completing a trial — it directly impacts data reliability, study timelines, budgets, and most importantly, patient outcomes.
Here, we explore the key barriers to retention and provide actionable strategies to improve engagement and outcomes in obesity and weight-management trials.
Why weight management trials face unique retention challenges
Obesity trials pose significant demands on patients, including long durations, sustained lifestyle changes and frequent monitoring. Beneath these more visible difficulties lie deeper human-centred challenges.
- Emotional load and stigma: The psychological toll of obesity, compounded by potentially difficult healthcare interactions, can leave patients feeling judged or misunderstood during trial visits.6 This can lower motivation and even hinder honest communication. Mental health challenges are especially prevalent in this population, and research shows that those experiencing anxiety or depression are at greater risk of dropping out early.2,7,8
- Intensive lifestyle demands: Maintaining restrictive diets, attending frequent appointments, or committing to regular exercise regimens, can feel overwhelming when balanced with work or family responsibilities.9 The attrition rate usually peaks at 6 months, as enthusiasm wanes and the demands become increasingly burdensome.1
- Unrealistic expectations: Social media may create inflated hopes about weight-loss outcomes, and when trial results don’t align with these expectations, particularly for patients in placebo groups, patients may feel disappointed and disheartened, leading to dropout.1,10
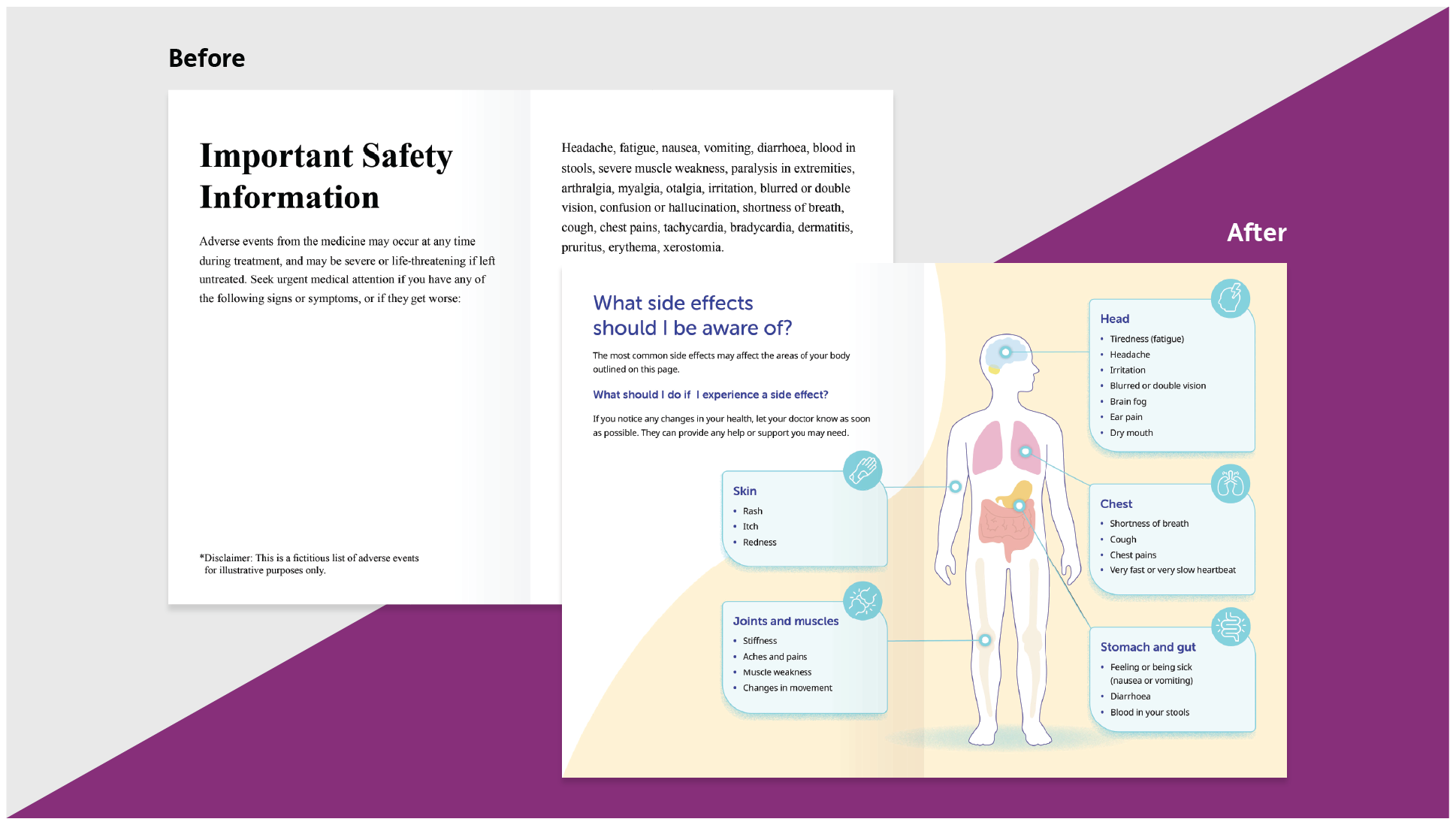
- Side effects: Pharmacological agents, including GLP-1 receptor agonists, often cause gastrointestinal side effects like nausea, vomiting, and diarrhoea, usually affecting between 40–70% of patients.11 These symptoms, especially during the dose escalation phase, can be demotivating and contribute to early dropout.
- Reporting fatigue: Trials often require detailed self-reporting of symptoms, diets, and behaviours. While crucial for data accuracy, this burden can feel cumbersome or intrusive. This data is also vulnerable to desirability bias, especially when patients feel self-conscious or stigmatised, leading to drops in retention and data quality.
Despite these challenges, research shows that proactive retention efforts can make a meaningful difference. Patients who engage in regular support sessions or enrol in patient support programs are significantly more likely to complete interventions.8,12 This highlights the importance of providing accessible, patient-centred support to improve retention outcomes.
Six strategies to support patients and improve retention
High dropout rates are not inevitable. By adopting simple yet impactful strategies, study teams can create a more supportive experience for patients.
1. Embed empathy into trial design
Retention begins with building trust through empathy. When trial staff communicate in a non-judgmental, empathetic way, the patient experience is drastically improved. For example, the use of positive language like “healthy lifestyle” instead of “weight-loss regimen” fosters a sense of support. Creating inclusive clinic environments, with accessible seating and parking, for example, can further ease patient concerns.
2. Lower the burden
Reduce logistical challenges by offering flexible scheduling, remote options, and transportation assistance. Providing modest compensation for time and travel also shows appreciation for patients’ efforts. These practices not only reduce friction but also lower barriers for underserved communities, improving overall retention.
3. Build in lifestyle support
Sustained lifestyle changes are inherently difficult. Access to dietitians or health coaches who provide culturally relevant guidance and encouragement can make a big difference.13 Pair this with user-friendly apps for tracking progress, communicating with coaches, and offering personalised tips. Structured, ongoing support has been shown to enhance completion rates.14
4. Motivate with milestones and value
Celebrating incremental achievements, such as reaching activity goals or completing a week’s food diary, helps sustain motivation. Providing feedback, even for patients in placebo groups, keeps them engaged. Monitor motivational levels and support site staff to identify early signs of disengagement through questionnaires or discussions. Equip sites with tools to reestablish motivation and reinforce the personal benefits of trial participation, like improved monitoring or contributing to future care.
5. Foster human connection
Assign each patient a dedicated point of contact for regular check-ins through text, phone, or email to foster a sense of reassurance and accountability. Self-monitoring programs tend to have the lowest adherence rates compared to supervised interventions.14 To manage urgent concerns, consider providing a 24/7 helpline for immediate support, helping patients feel supported, safe, and cared for.
6. Encourage peer and family engagement
Weight management often involves more than just the individual — it’s a shared journey. Build community through peer groups, buddy systems, or family-focused resources to create accountability and connection.14 For paediatric and adolescent trials, family involvement is especially critical.15,16
Shaping trials around the patient
Improving retention in weight management trials requires more than good protocol design — it calls for a deeper understanding of the patient experience and a holistic approach to supporting the person throughout their weight loss journey, not just during the trial itself.
By approaching trial participation with empathy, reducing logistical and emotional burdens, and offering meaningful, personalised support, sponsors and study teams can create an environment where patients feel respected, understood, and motivated to stay engaged.
A truly patient-centred approach not only strengthens retention and data quality but also delivers a more empowering and human experience for those who take part.
References
- Dalle Grave R, et al. Obes Facts. 2015;8(5):311–18.
- Ponzo V, et al. Eat Weight Disord. 2021;26(6):1729–36.
- Crichton GE, et al. Trials. 2012;13:111.
- Mirmiran P, et al. Int J Endocrinol Metab. 2021;19(3):e108170.
- Rodriguez PJ, et al. JAMA Netw Open. 2025;8(1):e2457349.
- Altamura M, et al. Front Psychol. 2018;9:2432.
- Sarwer DB, et al. Endocrinol Metab Clin North Am. 2016;45(3):677–88.
- Everitt JD, et al. J Hum Nutr Diet. 2023;36:1931–41.
- Toth-Capelli KM, et al. Health Promot Pract. 2012;14(3):441–50.
- Lindström D, et al. Contemp Clin Trials. 2010;31(1):22–6.
- Gorgojo-Martínez JJ, et al. J Clin Med. 2023;12(1):145.
- Wharton S, et al. Obes Sci Pract. 2020;6(4):382–9.
- Numan. Numan weight loss programme effectiveness. Available here. Accessed August 2025.
- Lemstra M, et al. Patient Prefer Adherence. 2016;10:1547–59.
- Ross LJ, et al. Int J Behav Nutr Phys Act. 2019;16:88.
- Lee K, et al. Nutrients. 2019;11(12):3046.